Summary – Balancing cost control, accelerated time-to-market and SaMD/cybersecurity regulations, MedTech players must rethink their architectures and care pathways around digital levers. Telemedicine and IoT enable continuous monitoring through connected devices and modular, open-source, microservices platforms compliant with FHIR/HL7 and FDA/MDR, while AI and MLOps workflows leverage and secure data.
Solution: define a pragmatic roadmap to iteratively deploy a modular, secure, ROI-focused stack that ensures scalability and compliance.
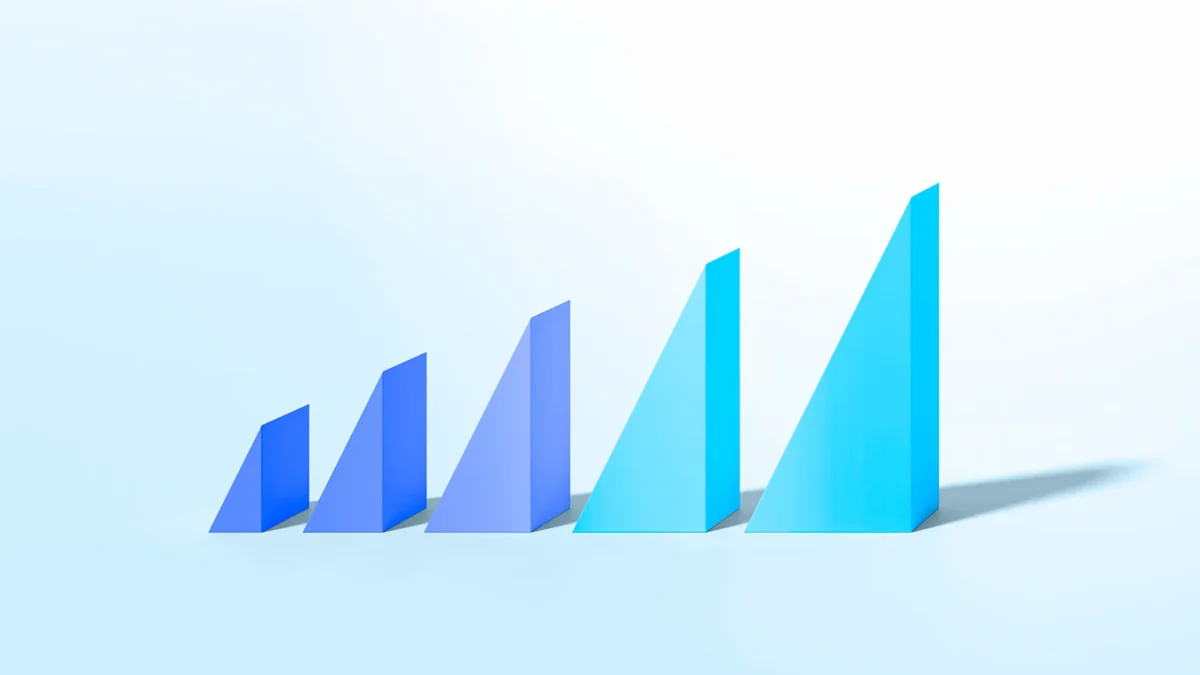
The MedTech sector, long characterized by its stability and controlled innovation cycles, now faces a dual constraint: managing costs while accelerating time-to-market in the face of new technological entrants. Regulations—particularly in cybersecurity and software as a medical device (SaMD)—are tightening, pushing organizations to rethink their architectures and business processes. In this context, digital transformation is no longer a choice but a strategic imperative.
This article explores how telemedicine, IoT and artificial intelligence can act as levers to reinvent care pathways, optimize data utilization and build robust, compliant digital ecosystems.
Telemedicine and IoT: reinventing care pathways
Telemedicine and IoT enable remote health services with continuous monitoring. These technologies provide the flexibility to reduce hospitalizations and improve patient quality of life.
The combination of connected medical devices and video-conferencing solutions paves the way for personalized patient follow-up, regardless of their location or mobility. Connected devices—such as glucometers, blood pressure monitors or activity trackers—transmit real-time data to secure platforms, offering a 360° view of patient health.
In this approach, the IT teams play a critical role: they must ensure network resilience, secure data exchanges and compliance with standards like FDA or European MDR. The architecture must be modular and scalable to accommodate new sensors without overhauling the entire system.
By leveraging open-source solutions and microservices, MedTech providers can minimize vendor lock-in and enable agile deployment of new teleconsultation features.
Home care and continuous monitoring
Home care relies on wearable devices and environmental sensors capable of detecting physiological or behavioral anomalies. Their major advantage is anticipating medical crises.
Successful deployment requires orchestrating data collection, validation and delivery to healthcare professionals almost instantaneously. Embedded algorithms—short data processes at the edge (edge computing)—optimize latency and safeguard sensitive information.
The modular network architecture makes it possible to add new sensors without disrupting the existing infrastructure. Standard protocols (MQTT, LwM2M) and certified cloud platforms are preferred, leveraging open-source building blocks to avoid technological lock-in.
Smooth communication between clinicians, patients and caregivers
Coordination among care stakeholders now relies on collaborative interfaces integrated into shared medical records (SMRs). These interfaces must be ergonomic and accessible on all device types.
Example: A mid-sized Swiss hospital implemented a secure messaging platform with a patient portal. This initiative demonstrated that a unified interface reduced redundant calls by 30% and improved protocol adherence.
Such a solution shows that clear governance of access rights and roles—administrator, clinician, patient—is essential for ensuring confidentiality and traceability of exchanges.
Security and reliability of IoT devices
Connected devices remain prime targets for attacks. It is imperative to encrypt data flows and enforce robust cryptographic key management policies.
OTA (Over-The-Air) updates must follow trust chains and digital signatures to prevent code injection. The architecture must be resilient, isolating compromised devices to ensure service continuity.
A centralized monitoring system with proactive alerts enables rapid detection and remediation of any performance or security anomaly.
Connected health platforms: orchestrating and enriching data
Connected health platforms aggregate heterogeneous streams from medical devices and applications. The main challenge is ensuring interoperability while maintaining regulatory compliance.
To meet these challenges, organizations rely on data buses and standardized APIs (FHIR, HL7) that facilitate exchange between diverse sources. Microservices ensure system scalability and resilience.
Leveraging this data requires a rigorous governance framework, combining validation workflows, granular access rights and regular audits. Compliance with GDPR, FDA 21 CFR Part 11 or European MDR is a prerequisite.
Open-source platforms paired with orchestrators like Kubernetes provide a flexible, cost-effective foundation that fosters innovation and component portability.
Aggregation and interoperability of streams
Data aggregation must handle various formats: continuous streams (IoT), batch files, real-time alerts. A dedicated ingestion engine ensures the consistency of incoming data.
Each data point is tagged with a timestamp, a signature and an origin identifier to guarantee traceability. Transformations (data mapping) are performed via decoupled modules, simplifying maintenance and the addition of new formats.
An orchestration layer oversees all data pipelines, automates quality tests and ensures a consistent SLA for each source type.
Enrichment through AI and machine learning
Machine learning algorithms detect clinical trends, predict exacerbations and optimize therapeutic dosages. They draw on anonymized, historicized datasets.
To ensure reliability, MLOps cycles are implemented: model versioning, performance testing, clinical validation and production monitoring. This iterative process limits drift and maintains compliance.
Scalability is achieved via serverless solutions or GPU clusters that scale automatically with load peaks, minimizing infrastructure costs.
Data governance and regulatory compliance
A health platform must meet strict confidentiality and traceability requirements. Implementing a unified data model simplifies audit and reporting.
Access rights are managed via RBAC (Role-Based Access Control), with periodic reviews and detailed logs for every critical action.
Regular penetration tests and third-party certifications (ISO 27001, SOC 2) boost user confidence and anticipate health authority requirements.
Edana: strategic digital partner in Switzerland
We support companies and organizations in their digital transformation
Big Data and augmented intelligence: leveraging silos to innovate
Analyzing data silos uncovers new business models and improves product quality. Augmented intelligence creates a competitive edge by anticipating needs.
Big Data solutions rely on data lakes or data warehouses, depending on real-time or batch processing needs. Opting for open-source technologies (Apache Kafka, Spark, Presto) ensures cost control and flexibility.
AI algorithms—regression, clustering, neural networks—depend on robust data-preparation pipelines built on automated, versioned ETL/ELT processes.
These approaches enable the development of predictive indicators, preventive maintenance services and R&D cost optimization by guiding clinical trials.
Value extraction and new business models
By transforming medical data into analytical services, MedTech players can offer analytics subscriptions, AI-assisted diagnostics or personalized therapy plans.
Each offering is built around documented, secure APIs, facilitating third-party integrations and the creation of partner ecosystem marketplaces.
This data monetization relies on a clear governance model that respects patient consent and current privacy regulations.
Optimizing product R&D
Data mining and statistical modeling accelerate protocol validation and rare side-effect detection. R&D teams thus receive faster feedback.
Lab experiments and clinical trials leverage digital twins, reducing time and cost of physical tests while improving accuracy.
Version traceability of models and datasets used preserves a complete audit trail for regulatory reviews.
Operational efficiency and predictive maintenance
Connected medical equipment generates logs and continuous performance metrics. Predictive maintenance algorithms anticipate failures before they impact service.
This approach lowers on-site support costs and service interruptions, while extending device lifespan.
Cloud-accessible analytics dashboards provide real-time visibility into fleet health and machine wellness indices.
UX, system integration and strategic partnerships: ensuring adoption and compliance
A user experience designed around clinical workflows drives adoption by professionals and patients. Partnerships streamline legacy system integration and enhance security.
Designing an intuitive interface requires precise mapping of business needs and regulatory constraints. Design cycles rely on prototypes tested in real settings.
Modernizing legacy systems involves a hybrid architecture: standardized connectors (FHIR, DICOM) link old software to new certified cloud platforms.
Alliances between MedTech players, specialized startups and open-source vendors create comprehensive ecosystems while controlling attack surface and vendor lock-in.
User-centered design and long product cycles
In MedTech, development cycles are often extended by clinical and regulatory validation phases. UX must anticipate these delays by delivering incremental updates.
User tests and co-creative workshops—including physicians, nurses and patients—ensure rapid tool adoption and limit redesign requests.
Agile governance, even within a certified context, facilitates gradual interface adaptation and reduces rejection risks.
Modernizing legacy systems
Legacy systems hold critical data and proven workflows. Complete overhaul is often operationally unfeasible.
The most effective strategy is to wrap these systems in APIs, gradually isolate critical modules and migrate new functions to a certified cloud platform.
This incremental approach minimizes risk, ensures service continuity and allows the integration of open-source components without disruption.
Hybrid ecosystems and strategic alliances
Technology partnerships expand service offerings while sharing R&D investments. They may cover AI components, homomorphic encryption solutions or strong authentication frameworks.
Each alliance is formalized by governance agreements and shared SLAs, ensuring clear responsibility allocation and regulatory compliance.
These collaborations demonstrate that open innovation and multi-actor cooperation are powerful levers to address MedTech’s business and legal challenges.
Turn regulatory pressure into a competitive advantage in MedTech
Digital transformation of medical devices and connected health services goes beyond mere technology integration. It requires a holistic strategy combining telemedicine, IoT, data platforms, AI, UX and partnerships. When orchestrated in a modular, open-source architecture, these levers reduce costs, speed up innovation and ensure compliance with the strictest standards.



 Views: 356
Views: 356